The Link between Age Related Macular Degeneration (AMD) and Sleep Apnea
AMD is an eye disease that affects people over 50, causing vision problems and possible blindness. In this article you will discover the link between AMD and sleep apnea. Sleep apnea is a common condition where breathing stops during sleep.

Introduction to AMD
AMD is a chronic, progressive, multifactorial disease that mainly affects people over the age of 50. It is an incurable disease in which vision deteriorates, leading to blindness. During normal vision, light enters the eye through the cornea, passes through the pupil and lens, and converges on the macula at the center of the retina (see Figure 1). When the macula is affected, the individual loses central vision, as illustrated in Figure 2. This loss of vision is often accompanied by difficulties in carrying out activities of daily living, and therefore influences the quality of life not only of those affected, but also of their loved ones.
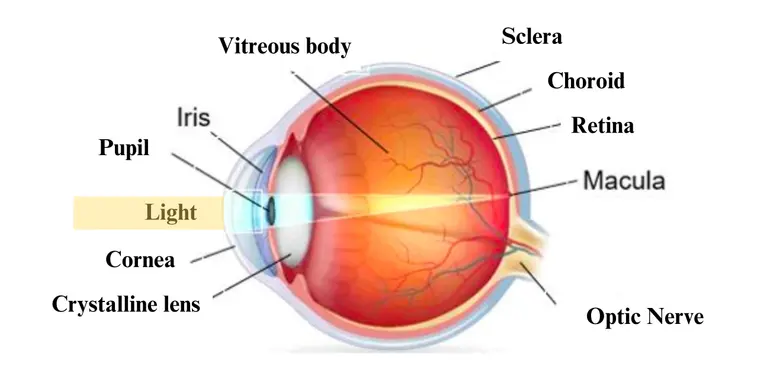
Figure 1. Anatomy of the human eye

Figure 2. Illustration of central vision loss in people with AMD
Exploring Sleep Apnea
Sleep apnea is a prevalent condition characterized by frequent interruptions in breathing during sleep, leading to insufficient oxygen intake by the body. If you exhibit symptoms like snoring, gasping, or other signs of poor-quality sleep such as excessive daytime sleepiness, it is advisable to consult your healthcare provider regarding sleep apnea.
There are two distinct types of sleep apnea:
- Obstructive sleep apnea (OSA) occurs when the upper airway experiences repeated blockages during sleep, resulting in decreased or complete cessation of airflow. ( Figure 3) This form of sleep apnea is the most commonly observed. Risk factors for obstructive sleep apnea include obesity, enlarged tonsils, hormonal changes, or anything that may narrow the airway.
- Central sleep apnea (CSA)arises when the brain fails to transmit the necessary signals for breathing. Underlying health conditions affecting the brain's control over the airway and chest muscles can lead to central sleep apnea.
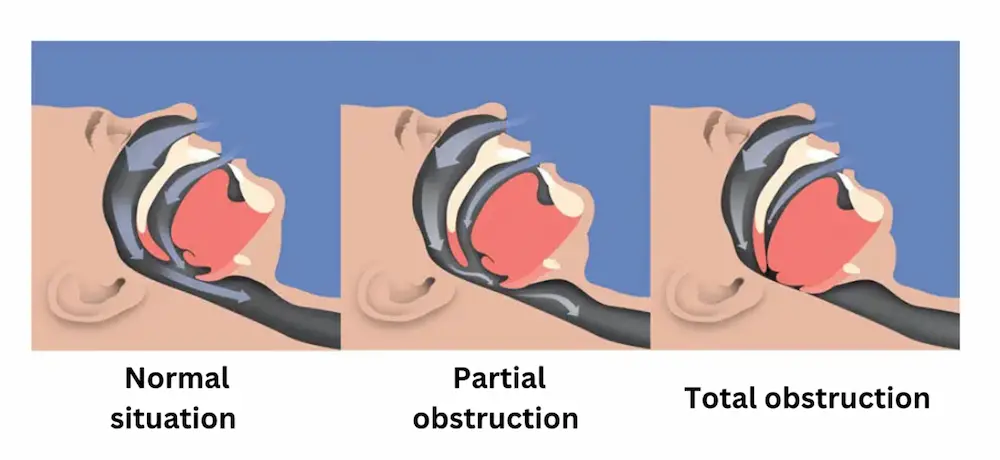
Figure 3. Illustration of obstructive sleep apnea
The Link between AMD and Sleep Apnea
There is a potential link between AMD and sleep apnea. Several mechanisms have been proposed to explain this connection:
- Oxygen Deprivation: Sleep apnea episodes can lead to intermittent drops in blood oxygen levels (hypoxia) due to reduced airflow. This hypoxia may contribute to retinal damage and the development or progression of AMD.
- Systemic Inflammation: Sleep apnea has been linked to chronic systemic inflammation. Inflammation plays a significant role in the pathogenesis of AMD, and the systemic inflammation associated with sleep apnea could potentially exacerbate retinal inflammation.
- Vascular Factors: Sleep apnea can cause vascular changes, including endothelial dysfunction and increased oxidative stress. These factors may impair blood flow to the retina, leading to the development of AMD.
Management and treatment methods
Continuous positive airway pressure (CPAP) is the main treatment for sleep apnea. Its use has been associated with improved visual acuity and reduced risk of progression in AMD patients with sleep apnea. Patients are encouraged to adopt a healthy lifestyle, including weight control, regular exercise and smoking cessation, can help mitigate the risks associated with AMD and sleep apnea. In addition, close cooperation between ophthalmologists, sleep medicine specialists and other healthcare providers is essential to ensure comprehensive care for patients suffering from both conditions.
Conclusion
AMD is a progressive disease that affects vision, while sleep apnea is a condition characterized by interrupted breathing during sleep. There is a potential link between AMD and sleep apnea due to factors such as oxygen deprivation, systemic inflammation, and vascular changes. Treatment for sleep apnea involves using continuous positive airway pressure (CPAP), which can benefit AMD patients. Adopting a healthy lifestyle and interdisciplinary collaboration among healthcare providers are essential for managing both conditions effectively.
Bibliography
- Wong WL, Su X, Li X, et al. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Health 2014.
- Mitchell P, Liew G, Gopinath B, Wong TY. Age-related macular degeneration. Lancet 2018.
- Mitchell J, Bradley C. Quality of life in age-related macular degeneration: a review of the literature. Health Qual Life Outcomes 2006.
- « What is sleep apnea ? | Nhlbi, nih » , NHLBI, NIH, 24 mars 2022.
- N. Website, « Sleep apnoea » , nhs.uk, 14 juin 2023.
- J. T. Sia et al., « Associations between age‐related macular degeneration and sleep dysfunction : a systematic review » , Clinical and Experimental Ophthalmology, août 2022.
- W. Y. Fang et al., « Role of sleep-disordered breathing in age-related macular degeneration » , BMJ open ophthalmology, mai 2023
- J. Lorenz, « Age-related macular degeneration associated with sleep dysfunction » , HCP Live, 29 août 2022.
- V. L. Pinto, « Continuous positive airway pressure » , StatPearls - NCBI Bookshelf, 25 juillet 2022.
- Merle BMJ, Colijn JM, Cougnard-Grégoire A, et al. Mediterranean Diet and Incidence of Advanced Age-Related Macular Degeneration: The EYE-RISK Consortium. Ophthalmology 2019.
- Delcourt C, Diaz JL, Ponton-Sanchez A, Papoz L. Smoking and age-related macular degeneration. The POLA Study. Pathologies Oculaires Liées à l’Age. Arch Ophthalmol 1998.
Age Related Macular Degeneration (AMD): Causes and Symptoms
AMD is a chronic eye disease that affects people over the age of 50, leading to vision loss and even blindness. There are two types: dry AMD and wet AMD, the latter being more severe. Early detection is crucial, as symptoms may not be apparent. In this article you can learn more about risk factors such as genetics, lifestyle and age.
The Link Between Diabetes and Age related macular degeneration: How to Protect Your Vision
In this article, we will explore the link between diabetes and Age related macular degeneration (AMD), what macular degeneration is, how it affects the eyes, prevention tips for diabetic macular edema, treatment options, lifestyle changes to protect your vision, and the importance of regular eye check-ups for diabetics.